New Imaging Technique Could Help with Future Alzheimer’s Diagnosis
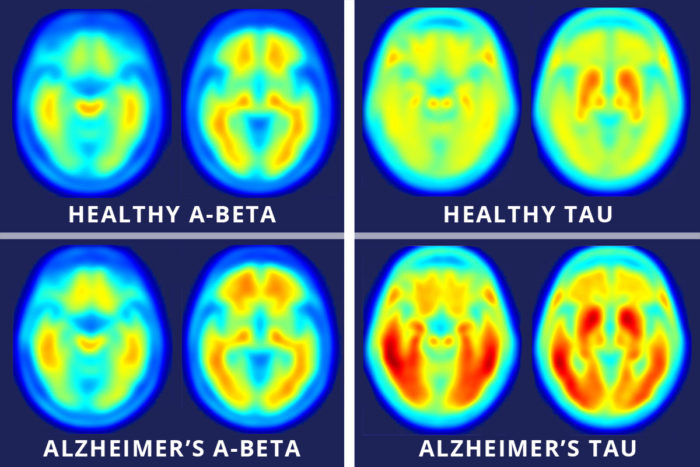 Globally, 47.5 million people are affected by Alzheimer’s disease and other forms of dementia. Alzheimer’s disease is characterized by the build-up of the proteins beta-amyloid and tau in the brain. Beta-amyloid plaque has been studied with the use of the positron emission tomography (PET) scan, while few methods have existed for scientists to study the build-up of tau protein. A recently published study in the Science Translational Medicine announced that new tau imaging agents will help scientists further study tau’s role in Alzheimer’s.
Globally, 47.5 million people are affected by Alzheimer’s disease and other forms of dementia. Alzheimer’s disease is characterized by the build-up of the proteins beta-amyloid and tau in the brain. Beta-amyloid plaque has been studied with the use of the positron emission tomography (PET) scan, while few methods have existed for scientists to study the build-up of tau protein. A recently published study in the Science Translational Medicine announced that new tau imaging agents will help scientists further study tau’s role in Alzheimer’s.
In a cognitively healthy individual, tau transports nutrients and energy along nerve fibers in the brain. When tau builds up, it breaks down into distorted strands that are no longer able to transport nutrients effectively. These twisted strands are known as neurofibrillary tangles, and these tangles have been closely linked with the onset and progression of Alzheimer’s disease.
Researchers from the Washington University in St. Louis tested the cognitive performance of 46 older adults and found that 36 were cognitively normal while ten had mild Alzheimer’s disease. They performed PET scans using the new tau imaging agents and found that cognitively normal participants had very few tau tangles, while the Alzheimer’s group had more tau tangles in the temporal lobe and cerebral cortex.
The research team also took cerebrospinal fluid measures of tau and found that these measures correlated more closely with tau deposition in the temporal lobe. Tau deposition in this area has been more closely linked to the status of dementia and is a better predictor of cognitive performance than beta-amyloid. The temporal lobe of the brain is heavily involved in sensory processing, visual memories, language comprehension and emotional understanding.
Overall, the study found that tau imaging predicts the status of Alzheimer’s disease more accurately than beta-amyloid imaging does. Previous studies have investigated the whole progression of Alzheimer’s disease in living participants using tau imaging. Beta-amyloid imaging, on the other hand, more accurately predicts the early disease state of Alzheimer’s and is a better diagnosis tool. The tau imaging tool, however, is still in the testing phase.
The Cognitive Therapeutics Method™ recommends eating a well-balanced diet, engaging in physical and mental activities, socializing and finding a sense of calm and purpose to help promote healthy brain functioning. Learn more about the method at www.CognitiveTherapeutics.com!
Sources

 Researchers from the University of Queensland in Brisbane, Australia, have discovered a new method to treat symptoms of Alzheimer’s disease in mice using ultrasound technology. The six-week study found that treating the mice with ultrasound waves resulted in a reduction of amyloid-beta plaque along with an improvement in cognitive performance.
Researchers from the University of Queensland in Brisbane, Australia, have discovered a new method to treat symptoms of Alzheimer’s disease in mice using ultrasound technology. The six-week study found that treating the mice with ultrasound waves resulted in a reduction of amyloid-beta plaque along with an improvement in cognitive performance.
 The study, published in the American Heart Association’s Journal Stroke, was conducted at the Kyoto University Graduate School of Medicine. Researchers assessed the balance of 1,387 adults with an average age of 67 by recording their one-leg standing time. The participants were asked to stand up and raise one leg in front of them, bent at the knee, for as long as they could. They repeated this on both legs twice, totaling two attempts per leg. All attempts were timed but only the best time for each leg was recorded. Participants were then given an MRI brain scan to identify any microbleeds or other abnormalities in the brain.
The study, published in the American Heart Association’s Journal Stroke, was conducted at the Kyoto University Graduate School of Medicine. Researchers assessed the balance of 1,387 adults with an average age of 67 by recording their one-leg standing time. The participants were asked to stand up and raise one leg in front of them, bent at the knee, for as long as they could. They repeated this on both legs twice, totaling two attempts per leg. All attempts were timed but only the best time for each leg was recorded. Participants were then given an MRI brain scan to identify any microbleeds or other abnormalities in the brain.